Is an Inpatient Stay Required for Your Treatment? Know When and How the Health Plan Covers It.
Dealing with a condition that might require an inpatient stay or hospitalization can feel like a lot to handle. It can become even more overwhelming to sort through the costs and what might be covered by the Health Plan. Fortunately, there are steps you can take before and during an inpatient stay that can help you make informed decisions about your care and help you to better understand what your out-of-pocket costs might be.
Before an Inpatient Stay
An inpatient stay at any facility requires pre-authorization from Anthem Blue Cross’ Utilization Management (UM) Department. You or your provider can initiate a request for pre-authorization by calling Anthem’s Pre-Authorization Review line at (800) 274-7767. For your convenience, this number is also listed on the back of your Health Plan ID card.
The UM department will determine whether an inpatient stay is the appropriate level of care for your condition based on established medical standards and nationally accepted clinical criteria and afterwards send a decision letter to both you and your provider. The letter will explain whether the requested number of days has been authorized, partially authorized or denied entirely. In addition, this letter will provide the clinical criteria that led to the UM decision and, if denied, provide you and your provider the next steps to appeal.
Regardless of the outcome, pre-authorization will help you better understand your out-of-pocket costs. If you are not pre-authorized for an inpatient stay or for the total number of days you requested, you still have the option of receiving care at the desired facility, with the understanding that you will be responsible for the cost of any days not pre-authorized by Anthem.
Example: Howard’s doctor has recommended he complete a 14-day inpatient detox at ABC Behavioral Health Center. The doctor contacted Anthem for pre-authorization and received authorization for 7 days at ABC. Howard begins his inpatient stay at the facility where only 7 days will be covered based on Anthem’s pre-authorization.
During an Inpatient Stay
If you have already begun an inpatient stay for which you have not obtained pre-authorization or if you are unsure whether you have obtained pre-authorization, make sure your provider has begun the pre-authorization process with Anthem’s UM Department. If you have obtained pre-authorization before your stay, be sure to keep track of how many pre-authorized days you have been granted. Staying beyond that time means you will be responsible for paying the full cost of your stay for all unauthorized days, and those costs will not be eligible for Health Plan reimbursement.
If you or your provider feels that you need to continue inpatient hospitalization beyond your pre-authorized time, you or your provider can request an extension of your stay from the Anthem UM Department. You may also request that your review be expedited, which could get you a decision within 24 to 72 hours.
A decision on your extension request—which may be a partial approval, alternative care options, full approval or denial—will be sent to both you and your provider. If you elect to stay past your pre-authorized number of days, even while waiting to hear the results of an extension request, you may be financially responsible for any days that were not authorized. If your extension request is approved, make sure to note the number of additional days granted in the extension to avoid paying the costs for exceeding your covered time.
Example: Howard received pre-authorization for 7 days of inpatient treatment at the ABC Behavioral Health Center. On day 5 of his stay, Howard’s doctor decides that Howard needs to complete the full 14-day detoxification treatment program on an inpatient basis and requests an extension of his inpatient stay from the Anthem UM Department. On day 7, Howard has not heard back from Anthem but decides to stay at ABC anyway. Howard learns on day 14 of his stay that his extension request was partially approved for 5 (instead of the requested 7) additional inpatient days with the recommendation that Howard transition to an intensive outpatient treatment center after the 5-day extension. In the end, Howard will be financially responsible for the additional 2 days of his stay that went beyond the approved 5-day extension and for any additional time that he elects to stay at ABC beyond the authorized extension.
I Don’t Agree with Anthem’s Decision. Now What?
You may request an appeal of any decision from Anthem’s UM department—including a denial of pre-authorization, a denial of an extension request, or a partial authorization of an extension. There may be up to three levels of review available to you.
- Your first level of appeal is with the Anthem Grievance and Appeal Department.
- If you do not agree with the decision of the Anthem Grievance and Appeal Department, you may then appeal directly to the Benefits Committee of the Health Plan’s Board of Trustees, who will consider all available materials previously presented, and any additional information you choose to submit.
- If you do not agree with the decision of the Benefits Committee, and the adverse determination involves medical judgment or a rescission of coverage, you may then request further external review by a contracted Independent Review Organization (IRO).
Making health-related decisions can be challenging, especially when you are determining whether to enter or continue inpatient treatment. The pre-authorization process is an excellent tool to help you navigate the treatment process and better understand your potential out-of-pocket expenses. If you have any questions, contact the Plans’ Participant Services department at (323) 866-2200, Ext. 401, or refer to the Health Plan Summary Plan Description for more information, available at www.dgaplans.org/health-plan-booklet.
My E.R. Visit Turned into a Hospital Admission. What Should I Do?
Inpatient stays can sometimes begin when an emergency room patient gets admitted into the hospital. If your stay begins this way, it is important to know that in a medical emergency, the Health Plan understands that pre-authorization may not be possible while prioritizing your immediate health situation. Instead, the required authorization can be requested during or even after your stay, though it is recommended that you or your doctor request authorization as soon as possible.
- Request or have the inpatient hospital request authorization for your inpatient stay from Anthem’s UM Department as soon as possible.
- If your initial review for authorization is denied—partially or entirely—you may file an appeal with Anthem’s Grievance and Appeal Department.
- If you do not agree with the decision of Anthem’s Grievance and Appeal Department, you and your provider can appeal directly with the Health Plan.


 OFFICE LOCATION & HOURS:
OFFICE LOCATION & HOURS: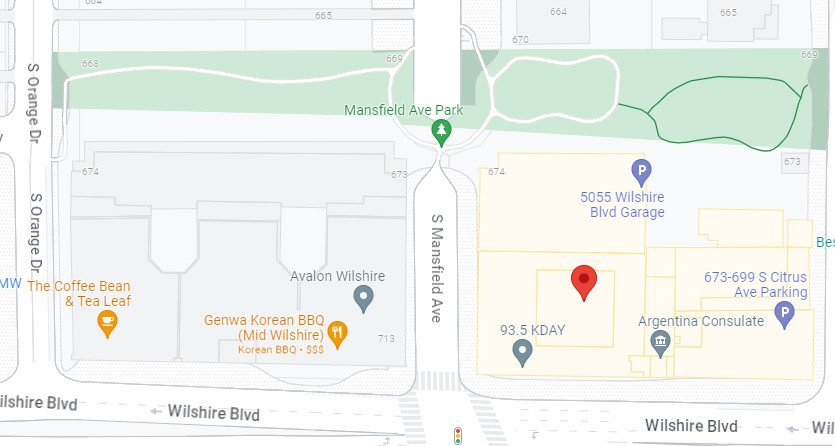
 MEETING INFORMATION:
MEETING INFORMATION: FAXES:
FAXES: