Health Plan Announces Changes to the Non-Network Claims Process and Payments
The Health Plan contracted with Green Light to improve how non-network claims are paid and how you are reimbursed. Unfortunately, it did not work as expected. The Board has approved changes to ensure you are reimbursed at the same rate as prior to the contract. Retroactive payments will be going out to those affected.
On January 16, 2024, the Health Plan partnered with Green Light Cost Management (“Green Light”) to help negotiate lower rates for non-network claims on behalf of Health Plan participants and protect them from balance billing whenever possible. Balance billing is when non-network providers charge participants for the billed amounts that exceed the maximum allowable charge under the Health Plan. In some cases, this can be thousands of dollars. When Green Light is able to negotiate pricing, you and the Health Plan benefit from lower pricing, and you receive protection from balance billing.
To assist Green Light with their negotiations with non-network providers, the Health Plan lowered the applicable benchmark for pricing non-network claims, called the Reasonable and Customary Charge, for non-network services. The maximum allowable charge for a non-network claim under the Health Plan is based on the Reasonable and Customary Charge amount.
In situations when non-network providers either: (1) require payment upfront, which is a common practice; or (2) refuse to further negotiate their billed amounts with Green Light, the reimbursement amount to participants can be lower based on the revised benchmark for determining the Reasonable and Customary Charge under the Health Plan, and participants are still not protected from balance billing in such cases. For these reasons, the Board of Trustees is making the following additional changes to the Health Plan to further protect participants in these scenarios. The changes will be retroactive to January 16, 2024.
-
How the Health Plan determines the Reasonable and Customary Charge has been revised
The maximum amount the Health Plan will reimburse you for a covered medical service rendered by a non-network provider is based on a benchmark called the Reasonable and Customary Charge. Previously, the Health Plan defined Reasonable and Customary Charge for non-network claims as the amount payable under the FAIR Health Index for the same or similar service in the applicable geographic area and would pay a maximum amount up to 80% of the FAIR Health rate*. After partnering with Green Light, the Health Plan amended the definition of Reasonable and Customary Charge to 150% of the Medicare reimbursement rate for that service, though there are exceptions.
Beginning January 16, 2024, the Reasonable and Customary Charge will be determined as follows:
-
The Health Plan will reimburse non-network claims at 80% of the FAIR Health standard under the circumstances below:
-
When you pay upfront and FAIR Health pricing exists; and
-
When Green Light negotiations with the provider are unsuccessful.
-
-
The Health Plan will use the 150% of Medicare reimbursement rate when a FAIR Health rate does not exist for the service provided.
-
When you have not paid your non-network provider upfront, Green Light will attempt to negotiate with your provider regarding your billed charges. If Green Light is successful in negotiating a better rate, you will be protected from balance billing, and you and the Health Plan will benefit from lower pricing.
Non-network providers will be prevented from balance billing you only when the claim has been successfully negotiated by Green Light. In all other cases, you may be subject to balance billing by the non-network provider. Whenever possible, you should have your non-network provider bill the Health Plan directly rather than making payment upfront. In situations when that is not possible, you should negotiate pricing before making an upfront payment.
-
When the Health Plan is not your primary plan, the Health Plan will begin by determining how much it would have paid had there been no other group coverage. Next it will find out what the primary plan paid. Then it will make a payment for the difference, if any, between the greater of the allowable amount and the amount paid by the primary plan, but not to exceed the amount the Health Plan would have paid if it was primary.
-
When there are Plan limits for a covered service (e.g., chiropractic and ambulatory services), the Health Plan will reimburse up to the Plan limit amount. See Article 1, Section 1 Visit and Benefit Amount Limitations of the Health Plan’s March 2025 Summary Plan Description for more information.
-
-
Additional payments will be made retroactively based on these changes.
These changes are effective retroactive to Green Light’s implementation on January 16, 2024. The Board of Trustees approved additional payments to participants and providers who received lower reimbursements than would have been paid as a result of these changes. Participants who are receiving an additional payment will also receive an updated EOB.
A non-network provider may receive additional payment if a claim meets all of the following four criteria: (1) the provider was not paid upfront; (2) the provider submitted the claim through the normal claims submission process directly to the Health Plan; (3) the provider was paid at the 150% of Medicare reimbursement rate; and (4) FAIR Health pricing exists for that service. If all four criteria are met, the provider will receive additional payment based on the new rules.
-
Green Light will continue to negotiate non-network claims that are not paid upfront.
Green Light’s successful negotiations with non-network providers continue to provide savings to both the Health Plan and participants. Whenever possible, Green Light will attempt to secure a lower price for non-network claims and agreement from the non-network provider to not balance bill you.
For details on the Health Plan’s partnership with Green Light, see https://www.dgaplans.org/greenlight.
*FAIR Health is an independent organization that compiles healthcare claims records from around the U.S. to provide cost estimates (based on geography) for most medical services.


 OFFICE LOCATION & HOURS:
OFFICE LOCATION & HOURS: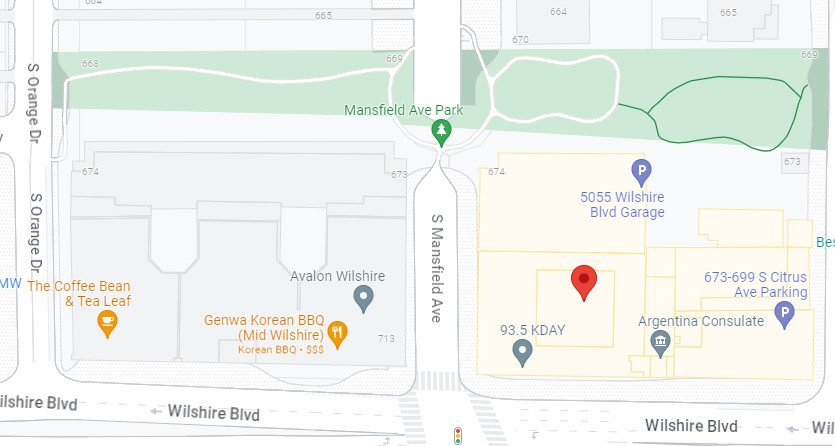
 MEETING INFORMATION:
MEETING INFORMATION: FAXES:
FAXES: