Introducing Palliative Care Benefits Effective October 1, 2022
 Effective October 1, 2022, the Directors Guild of America–Producer Health Plan (the “Health Plan”) will offer Palliative Care benefits to covered Health Plan participants and dependents. The new benefit will work in conjunction with the Health Plan’s medical benefits and be administered through the Motion Picture and Television Fund’s (MPTF) nationally and state recognized Palliative Care program. For more information about the new Palliative Care benefit or to find out if it might be helpful for you, call the MPTF Social Services Intake Line at (323) 634-3888.
Effective October 1, 2022, the Directors Guild of America–Producer Health Plan (the “Health Plan”) will offer Palliative Care benefits to covered Health Plan participants and dependents. The new benefit will work in conjunction with the Health Plan’s medical benefits and be administered through the Motion Picture and Television Fund’s (MPTF) nationally and state recognized Palliative Care program. For more information about the new Palliative Care benefit or to find out if it might be helpful for you, call the MPTF Social Services Intake Line at (323) 634-3888.
What is Palliative Care?
Palliative Care is a medical specialty that supports individuals with serious, chronic and life-threatening conditions at any stage of their illness. Unlike hospice care, which supports a patient solely at the end of life, Palliative Care supports patients throughout their illness and focuses not only on physical symptoms but also a person’s (and their family’s and caregivers’) mental, emotional and spiritual health. Palliative Care takes an interdisciplinary approach to assisting patients in every aspect of their lives, thereby improving their quality of life and aiding in their recovery.
Palliative Care has been shown to benefit patients, their families and caregivers in a number of ways, including reduced pain and suffering, reduced stress, reduced emergency room visits due to symptoms or worsening of the condition, and reduced use of post-acute care services, such as skilled nursing facilities.
What services will the Health Plan’s Palliative Care benefit cover?
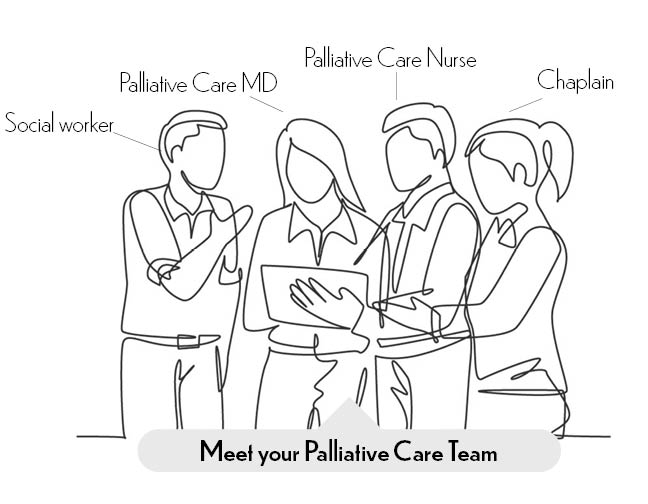
The Health Plan’s Palliative Care benefit comprises an added layer of support on top of the Health Plan’s medical benefit for those grappling with serious and chronic conditions. Through the Palliative Care benefit, participants can engage with the MPTF’s Palliative Care team—which can include a palliative care doctor, a registered nurse, a social worker and a chaplain—to coordinate the care necessary to address all of a patient’s needs throughout their illness…not just the medical ones.
The Palliative Care Team will work with the patient and/or their doctor to whatever degree the patient needs, whether that be a referral to a specialist, advice on treatment options or a trusted ear during an especially taxing day. Other than medical costs—which include deductibles, co-insurance and co-payment— covered Health Plan participants and dependents pay nothing for using the Palliative Care benefit.
Though each individual’s experience of Palliative Care will be different according to their need, the services available through the Palliative Care benefit can include:
- Access to a coordinated care team comprising a physician, RN, social worker and chaplain to work with you and/or your doctor at any point in your illness;
- Assistance with advance care planning;
- Assessments for depression, anxiety and other issues related to a diagnosis;
- Supportive counseling to assist you and your family in processing the changes a serious diagnosis can bring;
- Placements;
- Home health;
- Hospice;
- Support groups;
- Therapists;
- Durable Medical Equipment;
- Legal assistance;
- Food delivery programs;
- Caregiver support; and
- Bereavement support for family members and friends.
Any claims for services received from medical providers engaged through the Palliative Care benefit will be subject to Health Plan rules. The Health Plan’s deductibles, co-payments and co-insurance will apply.
Is Palliative Care right for me?
The Palliative Care benefit supports covered participants and dependents who are seriously ill. If during the last 12 months under your Health Plan coverage, you have had a medical claim with at least 1 qualifying diagnosis, the program may be right for you. The list below is not exhaustive.
Qualifying diagnoses:
- Alzheimer’s/dementia;
- Certain cancers;
- Cirrhosis;
- Heart failure;
- HIV;
- Lung failure/pulmonary illnesses;
- Neurodegenerative illnesses;
- Renal disease; or
- Stroke
Even if you believe you do not meet the criteria above or if you are not currently covered under the Health Plan, MPTF offers a range of supportive services to members of the entertainment community and their families. If you are unsure on whether you would be eligible for the Palliative Care benefit and would like an evaluation, contact the MPTF Social Services Intake directly at (323) 634-3888.
How do I get started?
You may be referred to the Palliative Care program by a provider, or you can get started by contacting the program yourself at (818) 876-1739. Though each person’s experience with Palliative Care will differ according to need, your experience will generally follow the three steps below:
-
- Phone assessment. You can call the Palliative Care program at (818) 876-1739, or if your provider has referred you to the program, you will be contacted by phone for intake by either the Palliative Care social worker or RN. During the intake call, the social worker or RN will ask questions about your circumstances including diagnosis, symptoms, support system, entertainment industry affiliation, military veteran status, advance care planning documents, etc. You will also receive a description of what Palliative Care is and how it might benefit your current situation.
- Initial visit (virtual or in person). The Palliative Care coordinator will reach out by phone to schedule your first visit with either the MPTF Palliative Care-certified team (social worker, chaplain, RN) alone or the MPTF team plus the UCLA Palliative Care, MD. The first visit is usually 60 minutes and may be, depending on your preference, via Zoom or in-person at the Palliative Care clinic on the MPTF’s Woodland Hills campus.
If a visit is going to include the UCLA Palliative Care MD, the Palliative Care RN will call you 1-2 days before your visit to get a list of the medications you are currently taking and note any specific symptoms or issues you want to address at the visit.
- Follow-up contacts, depending on need. Following a visit, the Palliative Care coordinator will reach out via phone to schedule the next visit. Follow-up visits are generally 30 minutes. Frequency of follow-up visits is dependent on your situation. The RN may call to follow up on any new medications or treatments that were prescribed and answer any questions. The social worker may call or email with information about resources mentioned during the meeting. The chaplain is available for any follow-up needs.