Request a Predetermination to Estimate Coverage
Requesting a voluntary predetermination helps you anticipate out-of-pocket costs
The Health Plan covers medically necessary visits, treatments and procedures for covered participants and their dependents. One of the Health Plan’s criteria for determining medical necessity includes whether the procedure or service is consistent with generally accepted medical guidelines and practices, which may require that certain treatment options be administered prior to or instead of others.
When standard medical practice is not followed, a treatment will be deemed not medically necessary and, therefore, will not be covered under the Health Plan. Doctors sometimes recommend immediate surgery, even though standard medical practice suggests utilizing non-surgical treatments prior to considering surgical intervention.
While you might assume that whatever treatment plan your doctor recommends is considered medically necessary under the Health Plan, this may not be the case if the treatment plan is not consistent with standard medical practices. If surgery is done and is later determined not to have been medically necessary, you may be held responsible for the full cost of the procedure, leaving you with significant unanticipated expenses.
For complex procedures and for procedures that include both reconstructive and cosmetic components, determining medical necessity is not straightforward. Although a surgery might seem like a single procedure, in reality, it might include several procedures, each of which must be evaluated for coverage by the Health Plan.
When in doubt, review each of the planned procedures with your doctor so you have a full understanding of your surgery and its costs. If you are uncertain about whether a treatment or procedure is medically necessary, you should request a voluntary predetermination from the Health Plan before receiving the service.
A predetermination will help you evaluate ahead of time whether the treatment is considered medically necessary and whether it will be covered.
WHAT IS A PREDETERMINATION?
A predetermination is a written analysis, provided by the Health Plan upon request, which evaluates the medical necessity of a particular procedure or treatment before you receive it. A predetermination will provide you with information on how the Health Plan might apply benefits for the service in question; however, it does not guarantee coverage. A final determination of coverage can be made only after the procedure has been performed, upon processing the claim and reviewing additional information and records submitted.
Examples of procedures for which a predetermination is especially recommended include (but are not limited to) orthopedic procedures (including various injections), bariatric surgery, varicose vein surgery, and nasal surgery.
A “predetermination” is not the same as a “pre-authorization.” Predetermination is a voluntary request for information from the Health Plan. Pre-authorization, on the other hand, is a required step your provider must take to confirm Health Plan coverage for certain services, including inpatient hospital stays, mental health and substance abuse intensive outpatient treatment, certain prescription drugs, partial hospitalization and residential care. In contrast to predetermination, pre-authorization guarantees that the authorized procedures will be covered.
HOW DO I SUBMIT A PREDETERMINATION REQUEST?
To start the predetermination process, you or your provider should submit your medical records and a letter of medical necessity, including diagnoses and procedure codes for the services being considered.
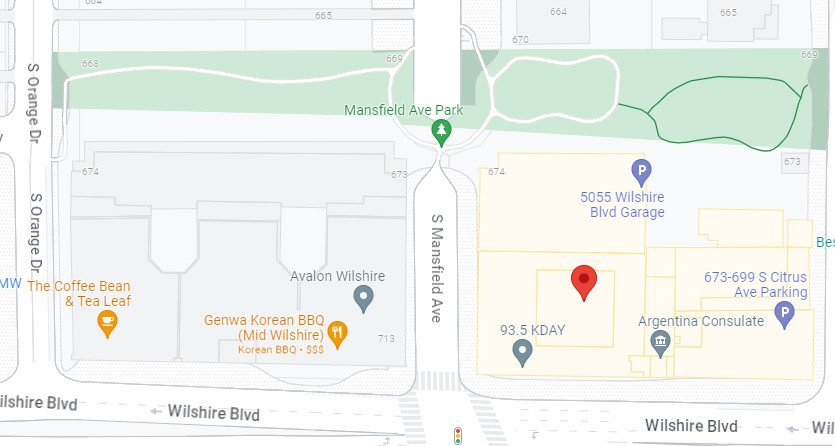
The request should be sent to the Health Plan Claims Department via fax at (323) 782-9287 or via email at hpclaims@dgaplans.org. Depending on the type of service in question, your predetermination may be sent to a third-party to conduct an independent medical review. Within 10 business days following receipt of your completed request, the Health Plan will send you or your provider a written response outlining the results of the predetermination of medical necessity for each procedure code.
The predetermination will indicate whether a particular procedure code reflects medical necessity; it is not a guarantee of coverage for the procedure. Please note that your predetermination applies only to the procedure codes submitted with your request.
For example, if you receive a predetermination of medical necessity for procedure codes 1, 2, and 3, and the actual claim submitted by your provider includes codes 1, 2, 3, 4 and 5, codes 4 and 5 may not be medically necessary, leaving you responsible for the costs of the procedures.
For any questions concerning predetermination, please call the Health Plan at (877) 866-2200, Ext. 401.